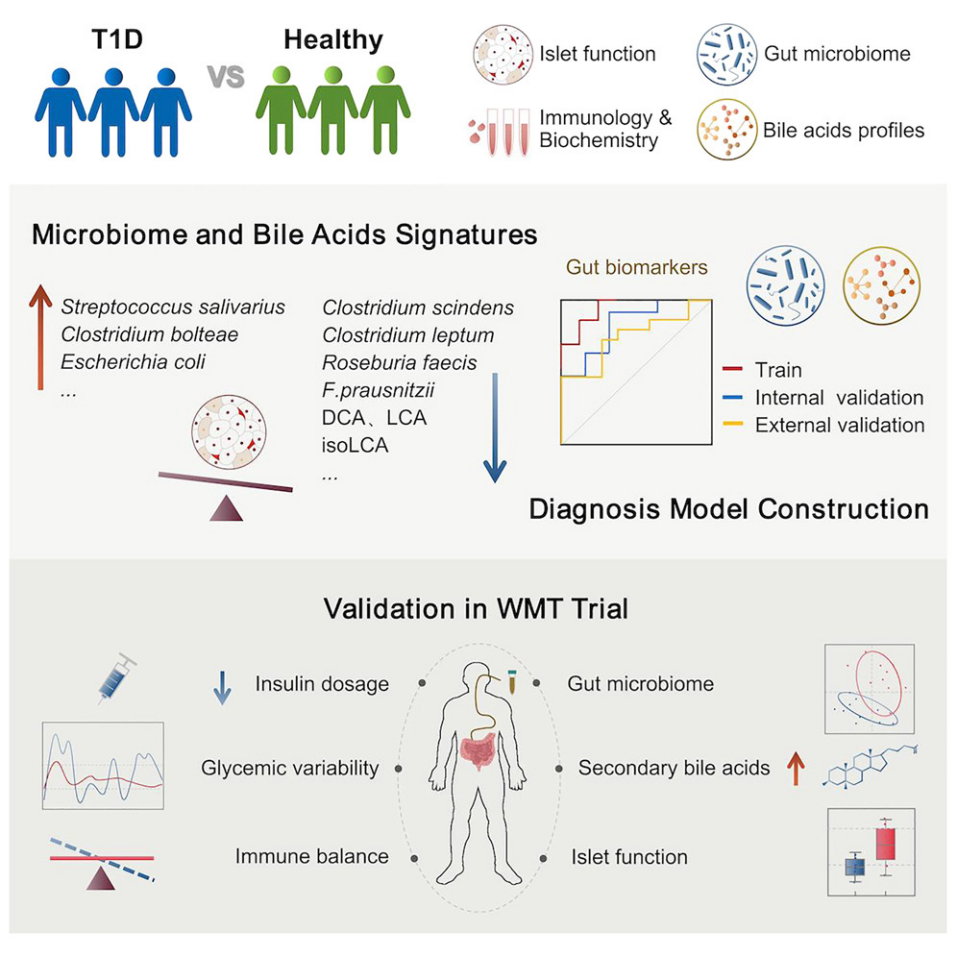
The international journal Cell Reports Medicine has published a groundbreaking study online by the research team led by Professor Yu Liu at Sir Run Run Hospital, Nanjing Medical University, titled Restoration of Intestinal Secondary Bile Acid Synthesis: A Potential Approach to Improve Pancreatic Beta-Cell Function in Type 1 Diabetes. This study reveals for the first time the dysregulation of gut microbiota and secondary bile acid metabolism in patients with Type 1 diabetes (T1D) and demonstrates that enhanced synthesis of secondary bile acids, particularly lithocholic acid (LCA) and isolithocholic acid (isoLCA), correlates with improved pancreatic beta-cell function following washed microbiota transplantation (WMT) in T1D patients. This breakthrough provides novel insights into the gut-pancreas axis mechanism underlying T1D pathogenesis and establishes a theoretical foundation for precision interventions targeting microbial-metabolite modulation.
The study found that T1D patients exhibit significantly reduced abundance of gut microbiota-associated pathways involved in secondary bile acid synthesis, leading to decreased levels of secondary bile acids such as deoxycholic acid (DCA), LCA, and isoLCA. Further analysis revealed a strong positive correlation between these bile acids and residual pancreatic beta-cell function. Innovatively, the team developed a microbiota-bile acid predictive model integrating five gut microbial biomarkers (e.g., Faecalibacterium prausnitzii and Roseburia faecis) and three secondary bile acids. This model outperformed single-omics models in training and validation cohorts (including an independent cohort) and effectively distinguished patients with preserved beta-cell function (T1Dpos) from those with beta-cell failure (T1Dneg), offering a novel tool for precise stratification.
Clinical translation studies demonstrated that WMT improved gut microbial ecology in T1D patients, reducing insulin requirements and glycemic fluctuations. Notably, post-WMT increases in intestinal LCA and isoLCA levels were significantly associated with enhanced beta-cell function in some patients, suggesting microbiota-derived metabolites as promising therapeutic targets. This study systematically elucidates the dynamic regulatory role of the gut microbiota-bile acid axis in T1D and advances the potential for personalized treatment strategies based on microbial-metabolic interactions, marking a critical step toward precision medicine in T1D management.
The study was co-authored by Qing Liu and Yifei Hua, Ph.D candidates at Sir Run Run Hospital, with corresponding authors Professor Yu Liu and Dr. Yangyang Li of Sir Run Run Hospital, and Professor Hao Wu of Fudan University’s Human Phenome Institute. Collaborative support was provided by Professor Yang Xiao’s team at the Second Xiangya Hospital of Central South University. This research was funded by the National Key Research Program and the National Natural Science Foundation of China.
Article Link: https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(25)00203-4
(Drafted by Yu Liu’s Research Team; Translation revised by Wu Wenbo)



